Here at DiscovHER HEALTH, we care about treating woman with PELVIC FLOOR DYSFUNCTION.
While the cause of PFD is not always known contributing factors may include pregnancy, vaginal delivery, pelvic trauma, stress, pelvic surgery and obesity.
While the cause of PFD is not always known contributing factors may include pregnancy, vaginal delivery, pelvic trauma, stress, pelvic surgery and obesity.
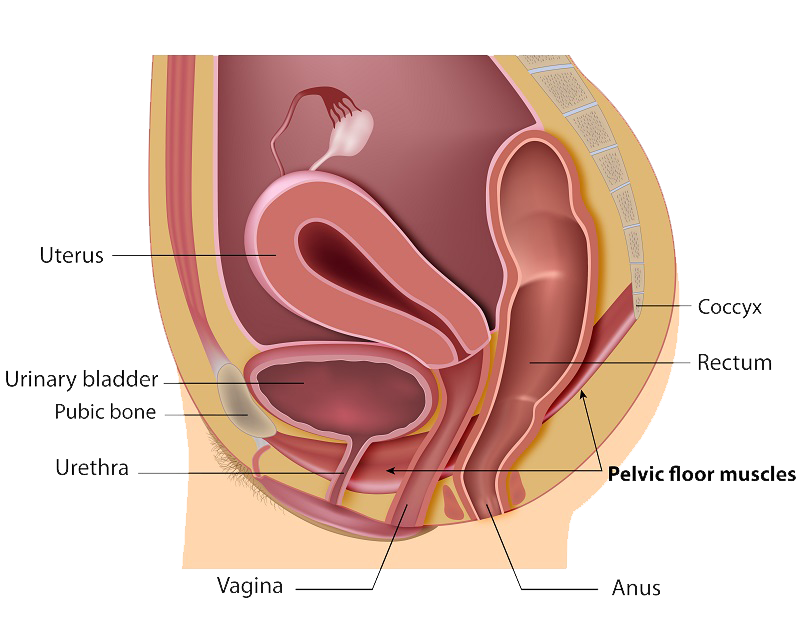
The pelvic floor consists of the bony pelvis (hip bones) together with different layers of muscles, fascia, and ligaments.
This intricate network acts like a hammock, supporting pelvic organs including the uterus, bladder, and rectum.
When these muscles become overactive, strained, or uncoordinated, they can cause pain in the pelvis, a common sign of pelvic floor dysfunction. This pain often leads the muscles to not contract, relax, or work together effectively, creating a cycle of discomfort and poor function.
PFD is also frequently found alongside pelvic diseases such as endometriosis, bladder pain syndrome, irritable bowel syndrome, overactive bladder, and vulvar pain. It can arise due to repeated straining, for example, with bowel movements, which leads to poor coordination of the pelvic floor muscles.
Additionally, the pelvic floor muscles may compensate for other musculoskeletal conditions, such as low back or hip pain, further contributing to pelvic floor dysfunction. Recognizing these connections is crucial for effective pelvic floor dysfunction treatment.
Identifying the symptoms of pelvic floor dysfunction is the first step toward finding relief and pelvic floor dysfunction treatment in Northern Virginia.
Understanding these signs empowers you to seek the right support for your pelvic floor dysfunction. Leaving these signs untreated can worsen conditions and impact your quality of life. Appropriate pelvic floor dysfunction treatment allows you to regain comfort, function, and confidence.
Physical Therapy is performed by a physical therapist who has been specifically trained in pelvic health. The physical therapist will perform a complete initial evaluation and, together with the patient, will establish goals and develop an individualized treatment plan.
A q-tip test (also called a cotton swab test) is done to diagnose vulvodynia. No speculum is required! Your health care provider may feel that other tests are necessary; these could include swabs to rule out infections or a biopsy to exclude skin conditions.
Learn More About the Q-Tip/ Cotton Swab Test
The treatment plan may include patient education, red light therapy, manual therapy, therapeutic exercise, postural training, breathing exercises, neuromuscular reeducation (teaching how to improve pelvic floor muscle control including relaxation, contraction, and coordination), biofeedback, and home exercise program.